careCycle Launches: Voice AI Teams for Medicare Agencies
"AI Teams That Scale Your Medicare Agency"
TL;DR: careCycle provides AI voice teams that handle the entire Medicare member journey, helping agencies greet members by first name 24/7, and provide a space to feel heard. In the process, they are tackling the industry’s single biggest problem: churn. Their early customers are achieving 37% better retention while saving thousands of agent hours.
Founded by Alex Doonanco & Evan Roubekas
Before founding careCycle, Alex led GTM at AI Rudder, a leading horizontal voice AI company.
He saw firsthand how generic AI solutions failed in highly regulated industries like Medicare. Agencies need purpose-built solutions that maintain strict compliance while delivering exceptional customer experiences.
Beyond expanding bandwidth for agencies, this technology allows them to invent new touch points previously unimaginable.
https://www.youtube.com/watch?v=ZZ-LbisGYpw
Medicare Agencies are Bleeding, and Seniors are Left in the Dark.
Medicare agencies face a devastating 50% annual member churn rate due to poor post-enrollment engagement. Licensed agents are forced to chase new sales instead of nurturing existing relationships, creating a vicious cycle that hurts both agencies and seniors.
It’s so bad that agencies they have spoken with actually lost money after selling thousands of policies in Q4 2024.
The Solution: Autonomous Member Care Teams that Make Seniors Feel Heard.
careCycle has built multi-agent AI teams that work together across the full customer journey:
Pre-Screening:
Because of increasingly aggressive marketing angles used to generate inbound calls, agencies drop hundred or thousands of inbound calls each day.
On top of this, agents spend previous time speaking with beneficiaries who might not be eligible or interested in their plan, who are at risk of being sold something they will cancel anyway.
careCycle takes calls 24/7, pre-screening callers, and seamlessly warm transferring to available licensed agents to assist them. If nobody’s available, they simply schedule an appointment that another AI team member automatically fulfills.
Post-Enrollment:
Their AI teams play a critical roll in keeping customers up to date on their policy application; something a shocking number of agencies don't have time to do.
In the process, they will provide them a space to feel heard and get any questions about their new plan answered.
After verifying the answer with a human-in-the-loop system, they deliver the message through another personalized and HIPAA complaint touchpoint.
Early Results
Since launching in Q4 2024, careCycle has:
- Helped a leading FMO write over $2M in renewals
- Talked with 50,000+ medicare beneficiaries
- Saved 4,000+ agent hours
- Achieved 5x increase in after-hours conversion rates
- Improved 90-day retention by 37%
Learn More
🌐 Visit carecycle.ai to learn more.
💫 Interested? Book a time to learn more here.
🤝 If you know: Medicare agency owners or executives, FMOs looking to provide better tooling for their agents, Healthcare compliance officers exploring AI solutions or Insurance industry professionals interested in contact center automation, reach out to the founders here.
🌟 Give careCycle a star on Github.
👣 Follow careCycle on LinkedIn.
Simplify Startup Finances Today
Take the stress out of bookkeeping, taxes, and tax credits with Fondo’s all-in-one accounting platform built for startups. Start saving time and money with our expert-backed solutions.
Get Started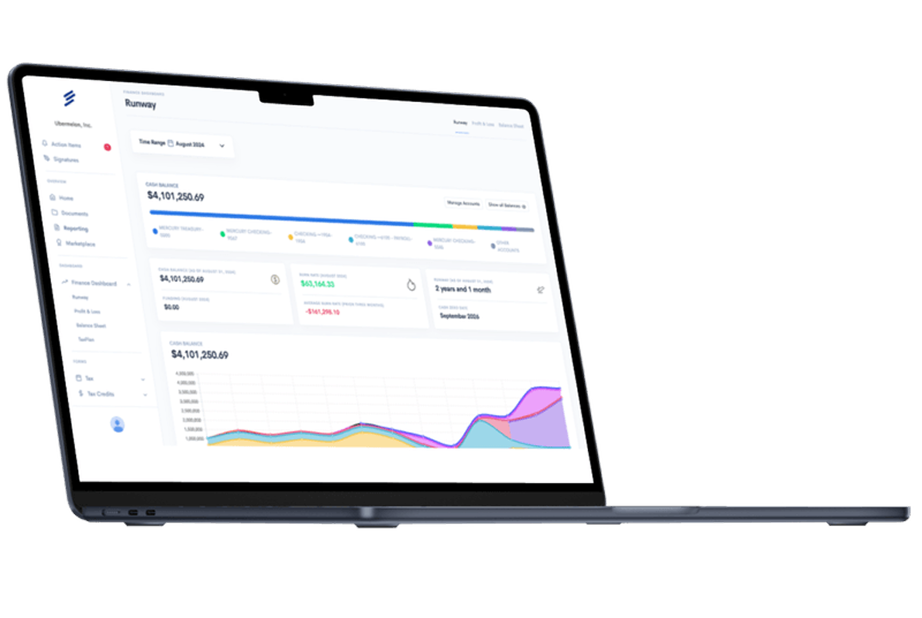









.png)









