Guardian AI Launches: Helping Healthcare Providers Fight Insurance Claim Denials
Guardian AI recently launched!
"Insurance companies are using AI to deny more claims than ever. Guardian gives providers the tools to fight back."
🛎 TL;DR After helping hospitals implement AI workflows at Palantir, the Guardian team has built a product to help healthcare providers automate how they manage insurance claim denials. This is desperately needed by the 40% of hospitals in the US that have negative operating margins each year. Within a month of launching, Guardian has helped recoup >$150,000 in claim value for providers.
Founded by Mayank Jain & Pranav Pillai
👨💼👨💼 The Team
Mayank and Pranav were two of the first members of Palantir’s Commercial Healthcare Team. They’ve worked together to improve hospital operations at Mount Sinai, HCA, NYC Health+Hospitals, and Cone Health.
After implementing AI programs at health systems the last several years, they look forward to democratizing AI across US healthcare and avoiding heartbreaking hospital and clinical practice closures.
🏥🚨 Hospitals are Dying
While Pranav was in college, the hospital where his mom worked in Philadelphia went bankrupt - Bernie Sanders actually picketed outside in protest.
During the last two years at Palantir, Mayank and Pranav worked with some of the biggest health systems in the country who, despite their size, had hundreds of millions in unpaid claims and were shutting down hospitals (see: Mount Sinai Beth Israel).
Insurance companies are using AI to deny more claims — the founders know this because, in their previous roles, they sat next to the team helping them do it. Guardian AI is on a mission to arm the providers and fix a system where 40% of hospitals are losing money.
🤖 Fighting Denials with AI
Denial management is a manual and painstaking process. Healthcare providers have a long string of tasks to complete — (1) call payers, (2) write appeal letters, (3) scrape patient charts for missing diagnoses and authorizations, (4) check for clerical errors, (5) check clearinghouses for patient eligibility and provider enrollment – the list goes on. There are so many tasks and systems required to work a denial that most healthcare providers end up writing off 5-20% of their accounts receivable.
The Guardian AI platform serves as a one-stop shop for denials management, where AI agents manage claims from end-to-end.

- Data Model: Guardian integrates with Clearinghouses, Payer Portals, and EHRs. Billing teams no longer have to switch between systems.
- Claim Status & Denial Cohorts: Looking at payer policies / contracts and trends in payer behavior, Guardian triages claims that are worth pursuing and determines a specific path to resolution.
- Automating Denial Resolution: Guardian's growing denial resolution suite automates payer phone calls, claim corrections and re-submissions, and a dozen other rote tasks in a denied claim’s lifecycle.
💰 Guardian AI's Offer:
They do risk-free, rapid denials + AR age assessments for hospitals and medical practices. Give Guardian AI your unpaid claims and they’ll run them through their software to find slam-dunk cases which payers have mis-processed — the founders have consistently found over $100K in low-hanging fruit when they’ve done this.
Learn More
🌐 Visit www.withguardian.ai to learn more.
🤝 Reach out to the founders via email or grab a time at withguardian.ai.
👣 Follow Guardian AI on LinkedIn.
Simplify Startup Finances Today
Take the stress out of bookkeeping, taxes, and tax credits with Fondo’s all-in-one accounting platform built for startups. Start saving time and money with our expert-backed solutions.
Get Started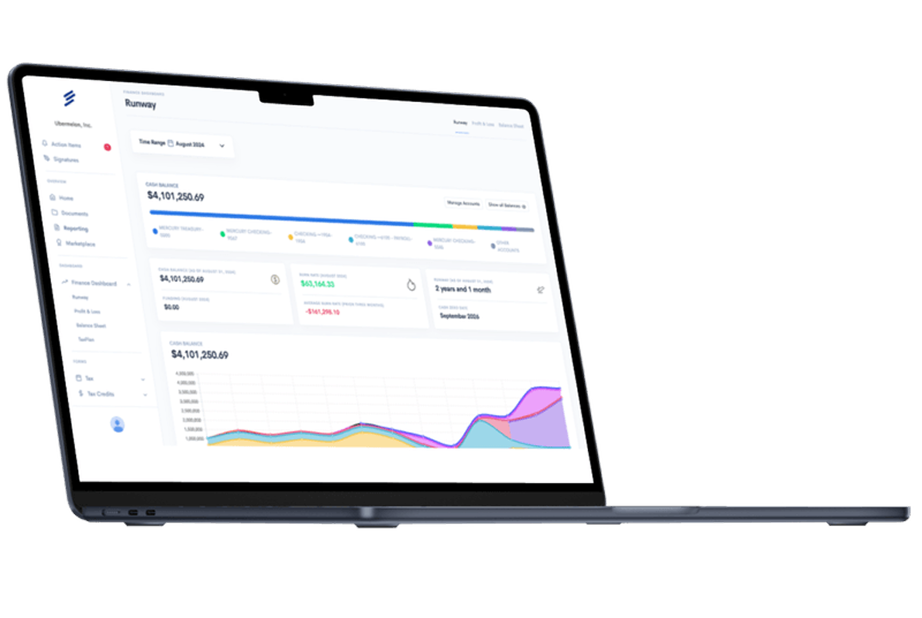









.png)









